Heart failure is the most common cause of hospitalization and death in the United States. At Yale New Haven Hospital (YNHH), the Risk EValuation And Its Impact on ClinicAL Decision Making and Outcomes in Heart Failure (REVEAL HF) clinical trial is currently underway to learn more about improving outcomes for these patients.
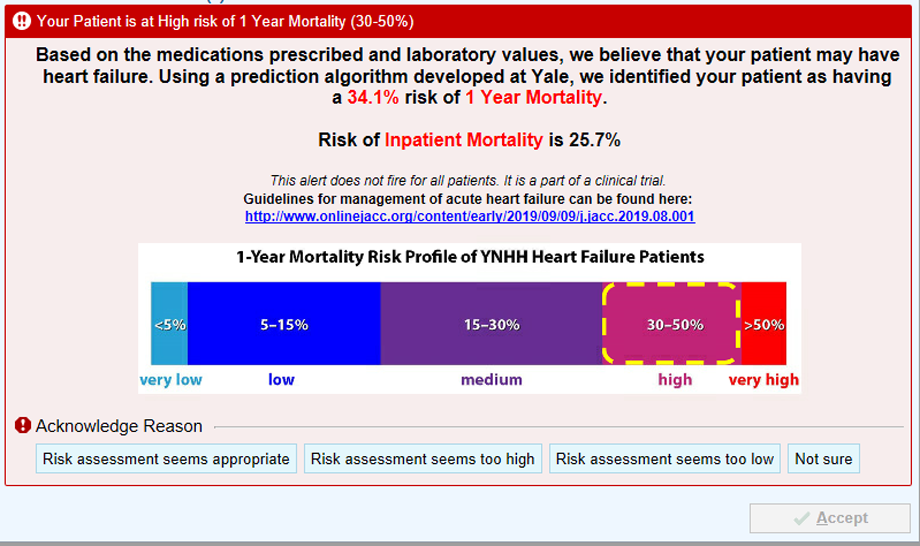
The trial is designed to assess whether giving care providers information about risk of inpatient and one-year mortality will improve care for patients with heart failure. The study utilizes a novel risk assessment tool, developed at Yale School of Medicine that is built into the patient’s electronic health record (EHR). The tool provides individual patient risk information on inpatient mortality and one-year mortality to caregivers in a randomized manner. The patient is eligible for the study if they meet a predetermined set of markers, such as elevated natriuretic peptide levels and administration of intravenous diuretics, that identifies them as likely to have heart failure.
Tariq Ahmad, MD, MPH, FACC and Nihar Desai, MD, MPH within the Section of Cardiovascular Medicine developed the trial, but needed additional expertise in embedding risk prediction algorithms within the EHR. They tapped the talents of the Program of Applied Translational Research, led by F. Perry Wilson, MD, MSCE, of the Section of Nephrology, who has run similar studies in the past. The trio all serve as co-principal investigators on the trial.
“Within the world of heart failure, innumerable risk scores have been developed, but no one has studied their impact on clinical decision making in a randomized clinical trial,” said Ahmad. “With Perry’s help, we created and validated algorithms based on patients from within Yale New Haven Health (YNHHS) that predict risk of inpatient and one-year mortality with a very high degree of sensitivity and specificity. Then, with the help of our incredible colleagues who lead medical informatics at YNHH, Nitu Kashyap, MD and Allen Hsiao, MD, we were able to embed the algorithms within the structure of a randomized clinical trial. Finally, we are able to get weekly results with the help of Richard Hintz at the Yale Center for Clinical Investigation. It has truly been the best kind of team science and a blueprint for pragmatic clinical trials at Yale.”
When a provider enters the EHR to place an order set (i.e. order bloodwork, a consultation, or medication), a graphic may display that informs the caregiver of the patient's risk of death during that hospitalization and at one-year post-discharge. They are also given a link to treatment for heart failure guidelines. Additionally, providers are asked to assess if the risk assessment given is too high, too low, or correct in their judgement.
The “special sauce” of the study, according to Wilson is randomization. “By randomizing which patients generate prognostic alerts, we can tell in an unbiased way whether the alerts change provider behaviors, and importantly, improve outcomes.” In an era of increasing electronic alerts, Wilson says, “we should not let new alerts into the wild without robust evaluation, ideally through a randomized trial.”
A live dashboard created by Ahmad and Desai tracks 30-day readmission rates of all heart failure patients, and other metrics such as use of guideline directed medical therapies, cardiology consults, defibrillator use, referrals for cardiac transplantation and left ventricular assist devices, and use of palliative care.
“Within our healthcare system, approximately 20% of people that are hospitalized for heart failure are readmitted within 30 days,” explained Ahmad. “The percentages are far higher for patients with higher risk. In fact, cases of advanced heart failure at Yale and across the country have a worse prognosis than most cancers. If this study can improve some of these outcomes, as we are hopeful it will, I think that we can make a very good case for having this be a part of the usual clinical care.”
“We're really interested about combining human and machine intelligence in medicine,” said Wilson. “There are clearly things that a human will pick up on that a machine can’t and vice versa. There is not a lot of research in this area, but in this trial, we have made it easy for providers to give us their intuition. It is going to be very interesting to see that if the combination of the computer and provider working together will make the best possible prediction. We look forward to assessing that too.”
“This study is a text book example of translational research, where we apply lessons from predictive analytics and decades of heart failure studies to the bedside of patients to improve their outcomes,” said Ahmad. “Yale should be at the leading edge of this work, which I think this study and several other projects in our pipeline will be doing.”
As of January 22, 2020, 177 patients have been enrolled on select floors of YNHH’s York Street Campus. Over the next few months, the team hopes to roll out this trial across all YNHHS hospitals in a step-wise fashion.
The REVEAL-HF trial encompasses expertise from across the Department of Internal Medicine. To learn more about the department, its mission, research and education initiatives, visit Internal Medicine.